ENDS Public Health: Difference between revisions
| Line 158: | Line 158: | ||
==Never Smokers== | ==Never Smokers== | ||
===2020: Electronic Cigarette Use Among U.S. Adults, 2018=== | |||
In 2018, 34 million U.S. adults were current smokers, and 55 million were former cigarette smokers for any duration (5). E-cigarette use was highest among current smokers and former smokers who quit cigarettes within the past year and those who quit 1–4 years ago. The percentages who had ever used an e-cigarette or who were current e-cigarette users declined among former smokers who had gone longer without smoking cigarettes and was lowest among those who never smoked cigarettes. | |||
===2017: Health impact of E-cigarettes: a prospective 3.5-year study of regular daily users who have never smoked=== | |||
In a small sample of young-adult never-smoking, daily EC users who were carefully followed for approximately 3½ years, we found no decrements in spirometric indices, development of respiratory symptoms, changes in markers of lung inflammation in exhaled air or findings of early lung damage on HRCT, when compared with a carefully matched group of never-smoking non-EC users. Even the heaviest EC users failed to exhibit any evidence of emerging lung injury as reflected in these physiologic, clinical or inflammatory measures. Moreover, no changes were noted in blood pressure or heart rate. Since the EC users who we studied were never smokers, potential confounding by inhalation of combustion products of tobacco were obviated. | |||
While the sample size was small, the results of this study may provide some preliminary evidence that long-term use of ECs is unlikely to raise significant health concerns in relatively young users | |||
===2016: Visible Vaping: E-Cigarettes and the Further Denormalization of Smoking=== | |||
Visible vaping was commonly reported by interviewees who typically interpreted such vaping as indicating that the individual was seeking to reduce or cease his or her smoking. Whilst the sight of someone using an e-cigarette could stimulate curiosity on the part of non-smokers as to what the experience of vaping was like there was little indication that our sample of non-smokers were intending taking up vaping on a regular basis. There were indications from our interviews that visible vaping had resulted in either no change in what individuals assessed as their likelihood of to smoke and for a minority of interviewees visible vaping had resulted in a reduced likelihood of smoking as assessed by interviewees. | |||
To the extent that electronic cigarette use remains distinguishable from smoking combustible cigarettes there is a possibility that vaping may be associated with further denormalization of smoking. | |||
==Pregnancy== | ==Pregnancy== | ||
Revision as of 22:18, 22 December 2020
Studies, Surveys, Papers, and Case Studies
- Sometimes it's necessary to view the PDF version to access the full study.
- This page is for referencing the possible benefits of ENDS products vs. smoking cigarettes from a Public Health standpoint. (Electronic Nicotine Delivery Systems are also known as vapor technology, ecigarettes, ecigs, EVP, etc.)
- If you'd prefer someone else to add a study to a topic, there is a subject section called "Suggested studies to add to this page". You may put the link in that section for one of the regular page editors to address.
- PAGE EDITORS - Please only add Studies, Surveys, Papers in this format to keep page consistent for all viewers.
- Topic
- Note here if animal study (leave blank if not)
- Year (list new to old) Name of Study (In link format to the study)
- Brief Summary
- Link to PDF Version
- Citation
- Acknowledgements (funded by, helped by)
- Keywords
- Other
Suggested studies to add to this page
2nd Hand Vapor
2018: Characterization of the Spatial and Temporal Dispersion Differences Between Exhaled E-Cigarette Mist and Cigarette Smoke
For both product categories, the particle concentrations registered following each puff were in the same order of magnitude. However, for e-cigarettes the particle concentration returned rapidly to background values within seconds; for conventional cigarettes it increased with successive puffs, returning to background levels after 30–45 minutes. Unlike for the e-cigarette devices tested, such temporal variation was dependent on the room ventilation rate. Particle size measurements showed that exhaled e-cigarette particles were smaller than those emitted during smoking conventional cigarettes and evaporated almost immediately after exhalation, thus affecting the removal of particles through evaporation rather than displacement by ventilation.
2017 Evaluation of Chemical Exposures at a Vape Shop
By: U.S. Department of Health and Human Services Centers for Disease Control and Prevention National Institute for Occupational Safety and Health We collected air samples for flavoring chemicals (diacetyl, 2,3-pentanedione, 2,3-hexanedione, acetaldehyde, and acetoin), nicotine, formaldehyde, and propylene glycol. Concentrations of vaping-related chemicals in our air samples were below occupational exposure limits.
2017 Dr. Michael Siegel - Vape Shop Air Sampling by California State Health Department Suggests that Second Hand Vape Exposure is Minimal
This study, although conducted under very high exposure conditions in a small, non-ventilated vape shop with many employees and customers vaping and clouds of vapor visible, did not document any dangerous levels of exposure to any hazardous chemical. Nicotine exposure was essentially non-existent. Formaldehyde exposure was no different than in many indoor and outdoor environments at baseline. Acetone, acetoin, other aldehydes, toluene, benzene, and xylene were not detected. Chemicals that have been associated with "popcorn lung" were also not detected by the standard method. This study adds to the evidence that under real-life conditions, "secondhand vaping" does not appear to pose any significant health risks.
2014: Peering through the mist: systematic review of what the chemistry of contaminants in electronic cigarettes tells us about health risks
Threshold Limit Values (TLVs), were conducted under “worst case” assumptions about both chemical content of aerosol and liquids as well as behavior of vapers. There was no evidence of potential for exposures of e-cigarette users to contaminants that are associated with risk to health at a level that would warrant attention if it were an involuntary workplace exposures. Exposures of bystanders are likely to be orders of magnitude less, and thus pose no apparent concern.
2012: Comparison of the effects of e-cigarette vapor and cigarette smoke on indoor air quality
Comparisons of pollutant concentrations were made between e-cigarette vapor and tobacco smoke samples. Pollutants included VOCs, carbonyls, PAHs, nicotine, TSNAs, and glycols. Non-cancer risk analysis revealed “No Significant Risk” of harm to human health for vapor samples from e-liquids. With regard to cancer risk analysis, no vapor sample from e-liquids exceeded the risk limit for either children or adults.
Continuum of Risk
2020: E-cigarettes and their impact on health: from pharmacology to clinical implications
Despite many areas of ambiguity, current evidence suggest that e-cigarettes are less harmful than combustible products, but this only applies to smokers who completely switched to e-cigarettes. Thus, e-cigarettes still hold a great potential to reduce incidences of tobacco-related diseases and could be a part of the strategy to reduce the damage caused by smoking. Therefore, mechanisms should be developed to protect young people from using e-cigarettes but support smokers in their decisions to quit smoking with e-cigarettes.
2020: The ethics of tobacco harm reduction: An analysis of e-cigarette availability from the perspectives of utilitarianism, bioethics, and public health ethics
Much evidence suggests e-cigarettes are substantially less harmful than combustible cigarettes. E-Cigarette Availability (ECA) involves making e-cigarettes available to allow smokers to switch to them, and informing smokers of the lower risks of e-cigarettes vis-à-vis smoking. First, ECA is supported by a public health ethics framework. ECA is a population-level intervention consistent with respecting individual autonomy by using the least restrictive means to accomplish public health goals, and it supports equity and justice. Second, ECA is supported by four principles that form a biomedical ethics framework. By reducing smokers' health risks and not harming them, ECA fulfills principles of beneficence and non-maleficence. Because ECA allows smokers to make informed health decisions for themselves, it fulfills the principle requiring respect for persons and their autonomy. ECA can also advance justice by providing a harm reduction alternative for disadvantaged groups that disproportionately bear the devastating consequences of smoking. Policies of differential taxation of cigarettes and e-cigarettes can facilitate adoption of less harmful alternatives by those economically disadvantaged. We conclude that public health and biomedical ethics frameworks are mutually reinforcing and supportive of ECA as a tobacco harm reduction strategy.
2018: Harm Minimization andTobacco Control: ReframingSocietal Views of Nicotine Use To Rapidly Save Lives
FDA’s Gottlieb & Zeller state: “Nicotine,though not benign, is not directly responsible for the tobacco-caused cancer, lung disease and heart disease that kill hundreds of thousands of Americans each year” Inhalation of the toxic smoke produced by combusting tobacco products,primarily cigarettes, is the overwhelming cause of tobacco-related disease and death in the United States and globally. A diverse class of alternative nicotine delivery systems (ANDS) has recently been developed that do notcombust tobacco and are substantially less harmful than cigarettes. ANDS have the potential to disrupt the 120-year dominance of the cigarette and challenge the field on how the tobacco pandemic could be reversed if nicotine is decoupled from lethal inhaled smoke. ANDS may provide a means to compete with, and even replace, combusted cigarette use, saving more lives more rapidly than previously possible. Most reviews of toxicological, clinical, and epidemiological evidence indicate that the chemicals found in e-cigarettes, when used as intended, are far fewer and well below levels seen in cigarette smoke Studies in humans have also documented improved physiological outcomes, including reduced blood pressure, improved lung function, andlower disease symptoms, among smokers who switched to e-cigarettes E-cigarettes are much less dependence-producing than are cigarettes The potential harm of e-cigarettes falls in the low range on the continuum
2017: Potential deaths averted in USA by replacing cigarettes with e-cigarettes
Compared with the Status Quo, replacement of cigarette by e-cigarette use over a 10-year period yields 6.6 million fewer premature deaths with 86.7 million fewer life years lost in the Optimistic Scenario. Under the Pessimistic Scenario, 1.6 million premature deaths are averted with 20.8 million fewer life years lost. The largest gains are among younger cohorts, with a 0.5 gain in average life expectancy projected for the age 15 years cohort in 2016. The tobacco control community has been divided regarding the role of e-cigarettes in tobacco control. Our projections show that a strategy of replacing cigarette smoking with vaping would yield substantial life year gains, even under pessimistic assumptions regarding cessation, initiation and relative harm.
2016: Obsolete tobacco control themes can be hazardous to public health: the need for updating views on absolute product risks and harm reduction
Implications of updating the leading themes for regulation, policymaking and advocacy in tobacco control are proposed as an important next step. A new reframing can align action plans to more powerfully and rapidly achieve population-level benefit and minimize harm to eliminate in our lifetime the use of the most deadly combustible tobacco products and thus prevent the premature deaths of 1 billion people projected to occur worldwide by 2100
2016: Withholding differential risk information on legal consumer nicotine/tobacco products: The public health ethics of health information quarantines
The straight-forward principles of harm reduction should be as uncontroversial for tobacco products as they are for alcohol, cars, air travel, children's clothing, sexual practices, electrical goods and other goods and activities. Concerns for some adverse public health effects of harm reduction products such as SLT (Smokeless Tobacco) and vape are reasonable and worth trying to minimize, but there is no current evidence that such products actually represent an imminent danger to public health overall. Efforts to discourage the use of tobacco/nicotine products need not be reduced, but should be done in a harm-proportionate way. Telling consumers that all product options are as bad as cigarettes is untrue and almost certainly as deadly for users as telling at-risk populations that condom use affords no protection.
2016: Ethical considerations of e-cigarette use for tobacco harm reduction
Current evidence suggests that e-cigarettes have the potential to make significant public health gains through their role as tobacco harm reduction devices. In clinical practice, physicians have an ethical duty to provide their patients with evidence-based comparative risk assessments to allow them to make informed choices with respect to their smoking status. At its core, the objective of the smoking cessation agenda should be to improve population health, which will likely require some concessions in the form of harm reduction. This entails a willingness to negotiate the tensions between utilitarian and liberal ethics in designing policy that upholds autonomy while protecting broader public health interests.
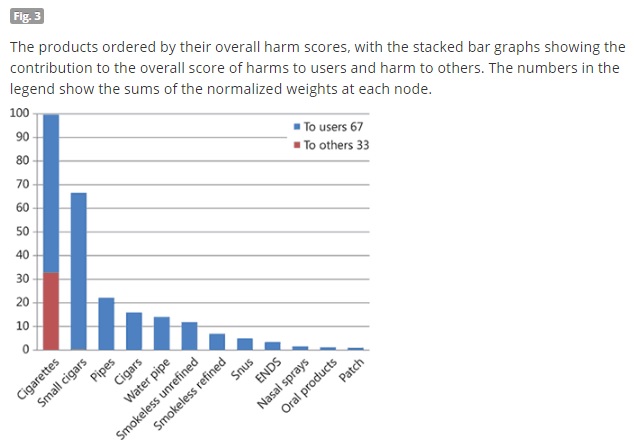
2014: Estimating the Harms of Nicotine-Containing Products Using the MCDA Approach
The group defined 12 products and 14 harm criteria. Seven criteria represented harms to the user, and the other seven indicated harms to others. The results of this study suggest that of all nicotine-containing products, cigarettes (and small cigars in the USA) are very much the most harmful. Interventions to reduce this pre-eminence are likely to bring significant benefits not just to users but also to non-smokers and society as a whole. Attempts to use other forms of nicotine such as ENDS and NRT to reduce cigarette smoking should be encouraged as the harms of these products are much lower.
Dependence (Addiction, Abuse) vs Harm / Harm Reduction - Ecigs and Nicotine
2020: Dependence on e‐cigarettes and cigarettes in a cross‐sectional study of US adults
Among current users, dependence on e‐cigarettes was significantly lower than dependence on cigarettes, in within‐subjects comparisons among dual users of both e‐cigarettes and cigarettes, and in separate groups of e‐cigarette users and cigarette smokers, and among both daily and non‐daily users of each product. Among former users, residual symptoms were significantly lower for e‐cigarettes than cigarettes, both among former dual users and among users of one product. The highest level of e‐cigarette dependence was among e‐cigarette users who had stopped smoking. Use of e‐cigarettes appears to be consistently associated with lower nicotine dependence than cigarette smoking.
2017: A comparison of nicotine dependence among exclusive E-cigarette and cigarette users in the PATH study
Cigarette smokers are more likely to consider themselves addicted, to have strong cravings, and to feel like they really needed to use their product. Cigarette smokers found it more difficult not to use in places where prohibited. E-cig users report less dependence on their product than cigarette smokers. E-cig users report a longer time-to-first-use after waking. These results are consistent with previous studies, in finding that exclusive daily e-cigarette users are less dependent on their respective product than comparable cigarette smokers.
2017: Evaluating nicotine dependence levels in e-cigarette users
Results showed that e-cigarette users scored lower than cigarette smokers in both FTND (Fagerström test for nicotine dependence) and all NDSS (nicotine dependence syndrome scale) subscales. Our findings extend previous research on e-cigarette use and nicotine addiction and suggest that e-cigarette users are less dependent on nicotine than current tobacco cigarette smokers.
2017: E-cigarettes: Impact of E-liquid Components and Device Characteristics on Nicotine Exposure
Given the large range of factors that can impact nicotine delivery, not only within the e-liquids but also in the hardware and user behavior, any regulatory framework intended to moderate nicotine exposure in users may not achieve its intended aim if it is solely limited to a regulation of the nicotine concentration of the e-liquid.
2014: Dependence levels in users of electronic cigarettes, nicotine gums and tobacco cigarettes
E-cigarettes may be as or less addictive than nicotine gums, which themselves are not very addictive.
2013: A fresh look at tobacco harm reduction: the case for the electronic cigarette
“Thus even if 50% of the non-smoking population should decide to addict itself to nicotine via an E-cig, the associated disease risks, if any, would be minimal. Thus, “abuse liability” is a moot point in this context.”
2012: Dependence on Tobacco and Nicotine Products: A Case for Product-Specific Assessment
Conclusion: “The other suggestion made is that when the totality of the dependence is measured, different forms of tobacco/nicotine products probably have different potential for dependence development. There might be a continuum of dependence where in one end, we find the cigarette and in the other end, NR products and particularly the patch formulation. If a particular product is far from cigarettes and close to NR on the continuum of harm and at the same time closer to cigarettes than NR on the continuum of dependence, this product may have considerable success in reducing the public health costs associated with cigarette use.”
2012: Clinical laboratory assessment of the abuse liability of an electronic cigarette
Electronic cigarettes can deliver clinically significant amounts of nicotine and reduce cigarette abstinence symptoms and appear to have lower potential for abuse relative to traditional tobacco cigarettes.
2011: Electronic cigarettes as a harm reduction strategy for tobacco control: A step forward or a repeat of past mistakes?
We conclude that electronic cigarettes show tremendous promise in the fight against tobacco-related morbidity and mortality. By dramatically expanding the potential for harm reduction strategies to achieve substantial health gains, they may fundamentally alter the tobacco harm reduction debate.
Elderly
2019 Article: New smoking statistics shows ‘gray vaping’ is on the rise in the UK
2019 PDF of Study (43 pages) NHS Statistics on Smoking
Mental Health
2020: E-cigarette use and associated factors among smokers with severe mental illness
Among participants, mean age was 46 years, the majority (70.3%) had tried an e-cigarette. Among those who had ever tried an e-cigarette, over half (54.6%) reported the reason was to quit smoking, while 13.9% reported that the reason was to reduce smoking.
2020: A qualitative study of the views about smoking, licensed cessation aids and e-cigarettes in people with schizophrenia spectrum disorders
There is a need to find ways of making traditional cigarettes less appealing and alternative less harmful nicotine products (licensed and unlicensed) more appealing and accessible to this group of high risk smokers.
2014: Use of e-cigarettes by individuals with mental health conditions
Individuals with mental health conditions (MHC) have disproportionately high tobacco-related morbidity and mortality due to high smoking prevalence rates. As high consumers of cigarettes, smokers with MHC may consider using e-cigarettes as an alternative form of nicotine delivery. Individuals with MHC were more likely to have tried e-cigarettes (14.8%) and to be current users of e-cigarettes (3.1%) than those without MHC (6.6% and 1.1%, respectively; p<0.01). Ever smokers with MHC were also more likely to have tried approved pharmacotherapy (52.2% vs 31.1%, p<0.01) and to be currently using these products (9.9% vs 3.5%, p<0.01) than those without MHC. Additionally, current smokers with MHC were more susceptible to future use of e-cigarettes than smokers without MHC (60.5% vs 45.3%, respectively, p<0.01). Smokers with MHC are differentially affected by the rise in popularity of e-cigarettes. Clinical interventions and policies for tobacco control on e-cigarettes should take into account the possible outcomes and their implications for this priority population.
2013: Impact of an Electronic Cigarette on Smoking Reduction and Cessation in Schizophrenic Smokers: A Prospective 12-Month Pilot Study
Even with intensive smoking cessation management programs specifically designed for patients with schizophrenia, quit rates are low. Although not formally regulated as a pharmaceutical product, the e-cigarette can help smokers with schizophrenia to reduce their cigarette consumption or remain abstinent and reduce the burden of smoking-related morbidity and mortality, particularly in schizophrenic patients who smoke
2011: Smoking Cessation with E-Cigarettes in Smokers with a Documented History of Depression and Recurring Relapses
The most important message from this case series is that these individuals were able to quit and to remain abstinent for at least 6 months after taking up an electronic cigarette. This is the first time that objective measures of smoking cessation are reported in smokers, suffering from depression, who quit after experimenting with the e-cigarette. This is quite outstanding in consideration of the fact that this result was accomplished by highly addicted smokers who repeatedly failed professional smoking cessation assistance without the support of recommended nicotine dependence treatments and smoking cessation counselling.
Never Smokers
2020: Electronic Cigarette Use Among U.S. Adults, 2018
In 2018, 34 million U.S. adults were current smokers, and 55 million were former cigarette smokers for any duration (5). E-cigarette use was highest among current smokers and former smokers who quit cigarettes within the past year and those who quit 1–4 years ago. The percentages who had ever used an e-cigarette or who were current e-cigarette users declined among former smokers who had gone longer without smoking cigarettes and was lowest among those who never smoked cigarettes.
2017: Health impact of E-cigarettes: a prospective 3.5-year study of regular daily users who have never smoked
In a small sample of young-adult never-smoking, daily EC users who were carefully followed for approximately 3½ years, we found no decrements in spirometric indices, development of respiratory symptoms, changes in markers of lung inflammation in exhaled air or findings of early lung damage on HRCT, when compared with a carefully matched group of never-smoking non-EC users. Even the heaviest EC users failed to exhibit any evidence of emerging lung injury as reflected in these physiologic, clinical or inflammatory measures. Moreover, no changes were noted in blood pressure or heart rate. Since the EC users who we studied were never smokers, potential confounding by inhalation of combustion products of tobacco were obviated. While the sample size was small, the results of this study may provide some preliminary evidence that long-term use of ECs is unlikely to raise significant health concerns in relatively young users
2016: Visible Vaping: E-Cigarettes and the Further Denormalization of Smoking
Visible vaping was commonly reported by interviewees who typically interpreted such vaping as indicating that the individual was seeking to reduce or cease his or her smoking. Whilst the sight of someone using an e-cigarette could stimulate curiosity on the part of non-smokers as to what the experience of vaping was like there was little indication that our sample of non-smokers were intending taking up vaping on a regular basis. There were indications from our interviews that visible vaping had resulted in either no change in what individuals assessed as their likelihood of to smoke and for a minority of interviewees visible vaping had resulted in a reduced likelihood of smoking as assessed by interviewees. To the extent that electronic cigarette use remains distinguishable from smoking combustible cigarettes there is a possibility that vaping may be associated with further denormalization of smoking.
Pregnancy
Perception - safety vs harm - effects on use
Propylene Glycol
Weight
- Click on the category link below for more studies by topic on ENDS and Nicotine.